This month, our colleague Olivia Taylor discusses the imaging of sub-acute and chronic ischemic brain lesions, based on two clinical cases received by the VEDIM team.
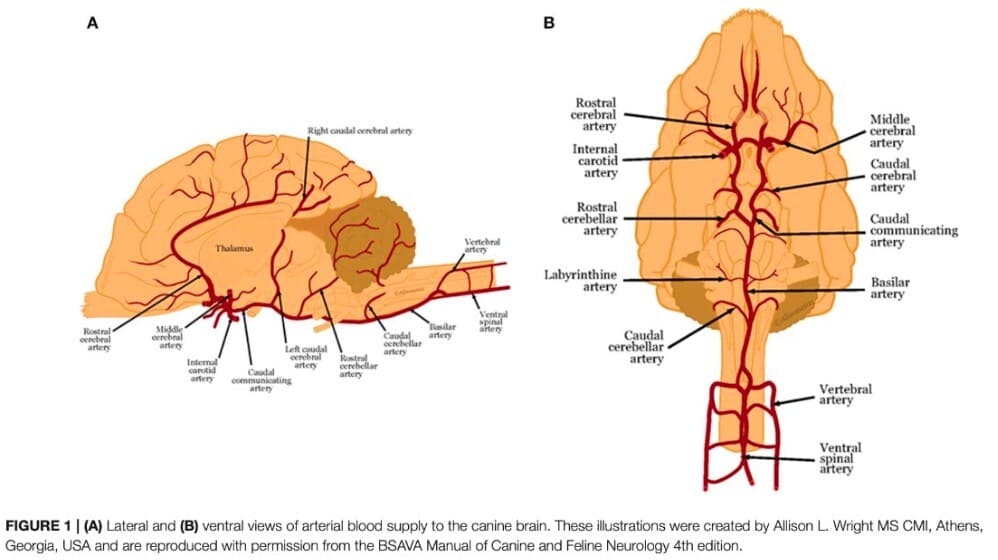
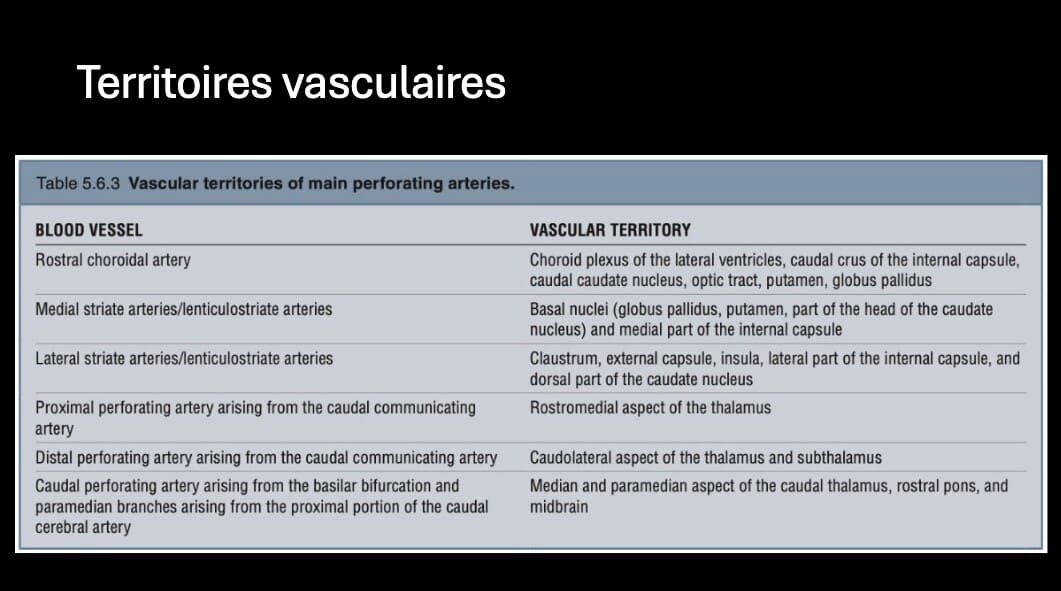
Ischemic brain injury results from vascular obstruction by an embolus from another vessel or from the heart, or from thrombosis forming locally. It manifests as an acute, non-progressive onset of focal neurological deficit. Hypoxia initially causes cytotoxic edema, followed by infarction of the hypoxia zone, and after 24 hours, vasogenic edema following rupture of the hematomeningeal barrier. Predisposing causes in our pets are mainly Cushing’s disease and chronic kidney disease. Lesions mainly affect the gray matter, and are located in specific territories of the arterial network of the brain, most frequently in the territory of the rostral cerebellar arteries.

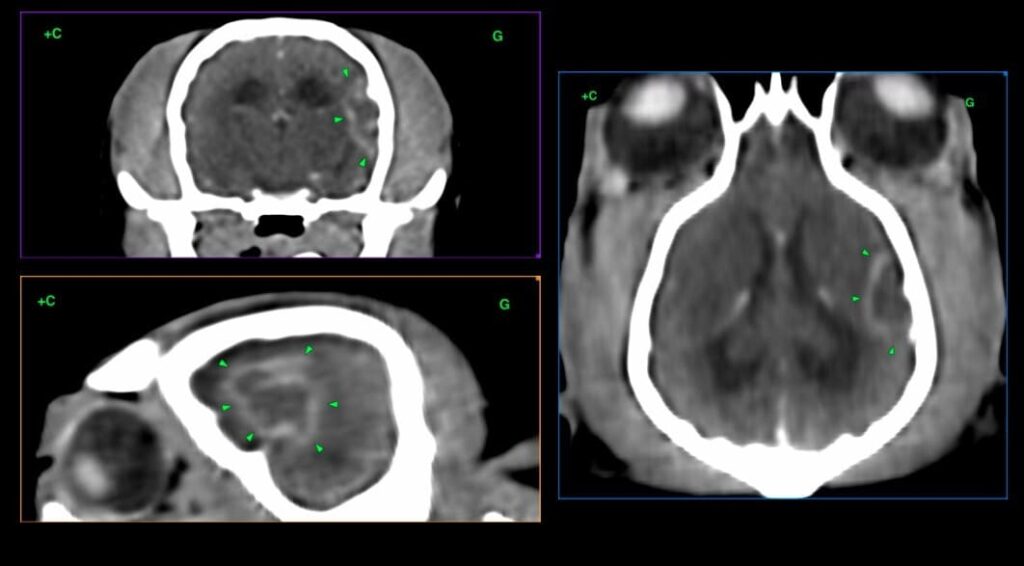
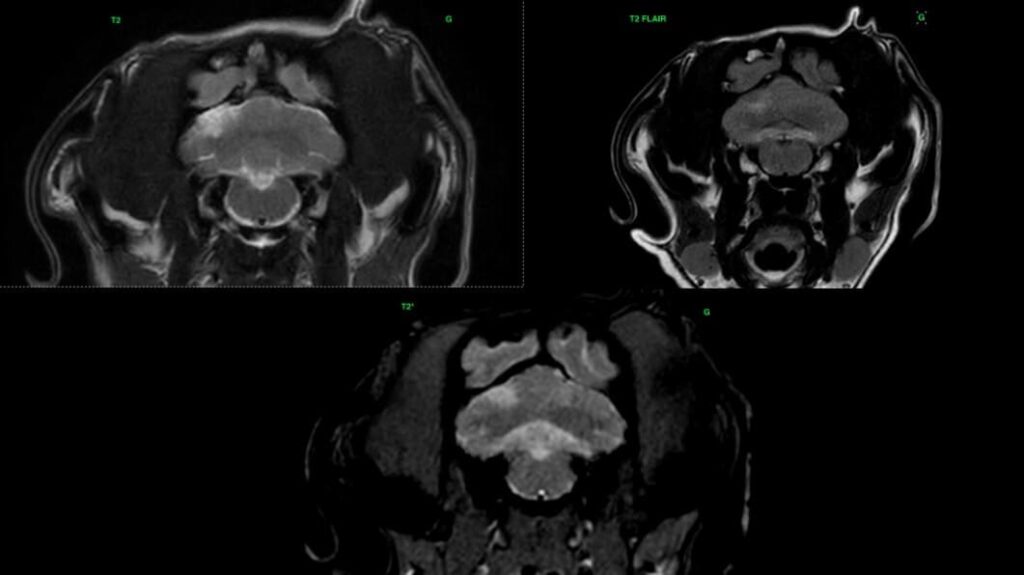
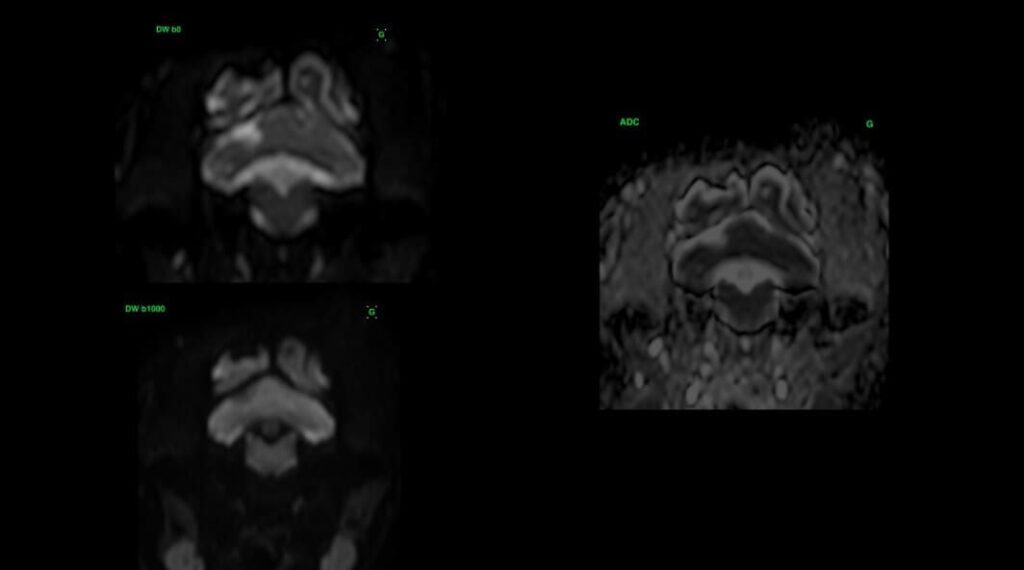
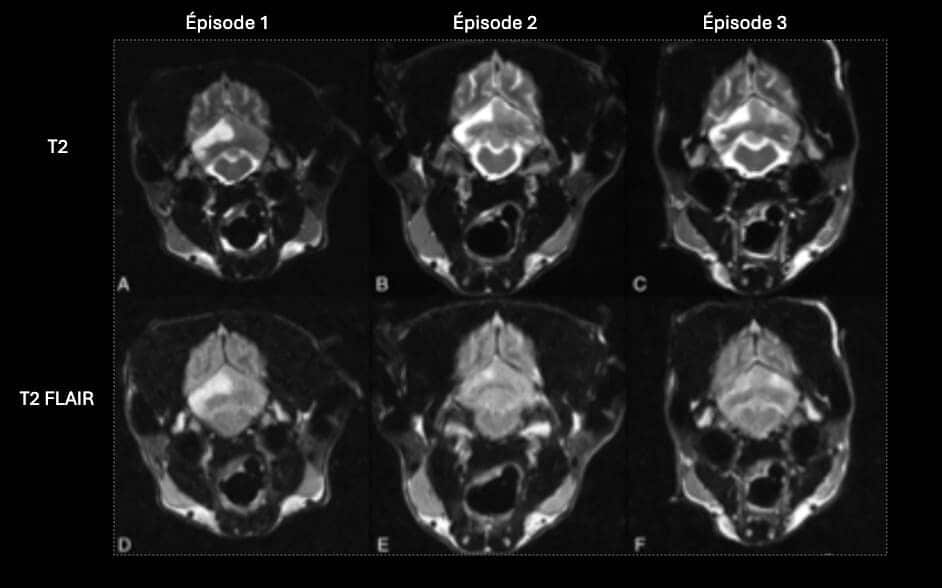
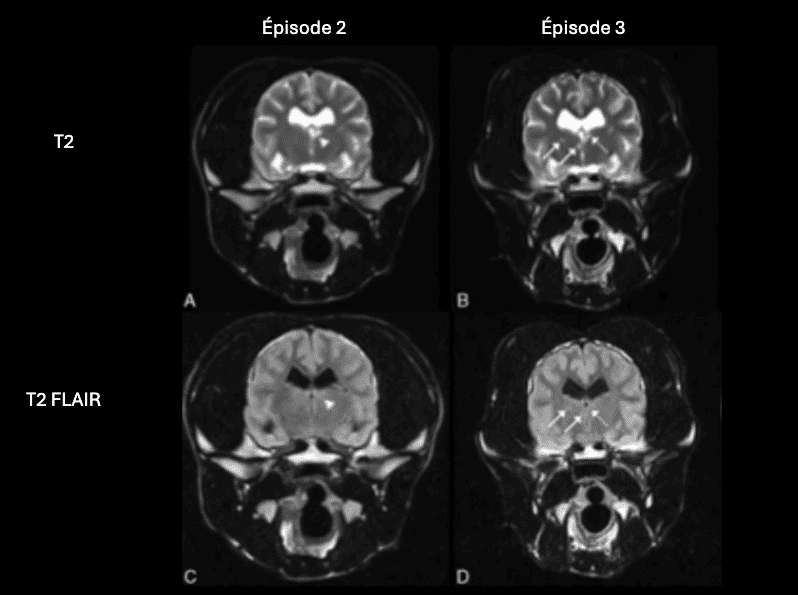
MRI is the imaging of choice for these ischemic lesions. Acute lesions appear hyperintense on T2 and T2 FLAIR sequences, hypointense on T1 weighting, and show no enhancement. Diffusion imaging enables earlier detection of these lesions. It can also be used to estimate the age of the lesion and the size of the infarcted nucleus. Acute lesions show diffusion signal restriction, and appear hyperintense on the DWI sequence, and hypointense on the ADC map. Values on the ADC sequence decrease for 4-5 days, normalize between 4 and 10 days, and increase again after 10 days. These lesions do not create a mass effect, except in the case of associated vasogenic edema, which peaks 3-4 days after lesion appearance. Peripheral enhancement of the lesion can sometimes be observed during the phase of rupture of the hematomeningeal barrier.
In the chronic phase, the T2 signal remains stable, but there is a progressive reduction in the T2 FLAIR signal. The signal is sometimes mixed on the T2 FLAIR sequence, due to the presence of hypointense areas of encephalomalacia and hyperintense areas of gliosis. Lesion size decreases in the chronic phase, with atrophy of the cerebral parenchyma. Any enhancement that may be present disappears when the hematomeningeal barrier is restored.


Clinical case 1 – “Isis” CT scan – subacute ischemic lesion in the middle cerebral artery territory